What does having a “Healthy Relationship to Food” actually look like?
I often talk about having a healthy relationship to food, as ultimately that’s what the end goal is for everyone I’ve worked with, but what does that actually mean?⠀⠀⠀⠀ ⠀ ⠀⠀
Oftentimes, it’s easy for people to see why dieting has failed them. They understand that they’ve hit “diet rock bottom”, how it’s affected them, and realized that it simply doesn’t work and can’t even FATHOM going on another diet. But other times dieting, labeling food, and eating according to external reasons, not what their body is telling them, is maybe all you know and what you’re used to. So it can be hard to envision what having a healthy relationship to food may actually feel like or look like. Especially given the amount of people I’ve met that unfortunately were put on their first diet at age 10 or less (!).
Well, let’s start with the opposite – an unhealthy relationship to food. What does that mean?
An unhealthy relationship to food can include any amount of the following, which often are considered “disordered eating behaviors”:
- stress and anxiety eating certain foods
- food guilt, views foods as “good” vs. “bad”
- skipping meals
- inflexible with food choices
- has firm food rules
- engages in trying different fad diets and rigid meal plans
- restricting food intake
- poor body image
- eats based on external rules instead of internal cues
- cutting out multiple foods and food groups without medical necessity
- thinking about food 24/7
- overexercising to make up for “bad” foods eaten
- meticulously planning your meals and snacks

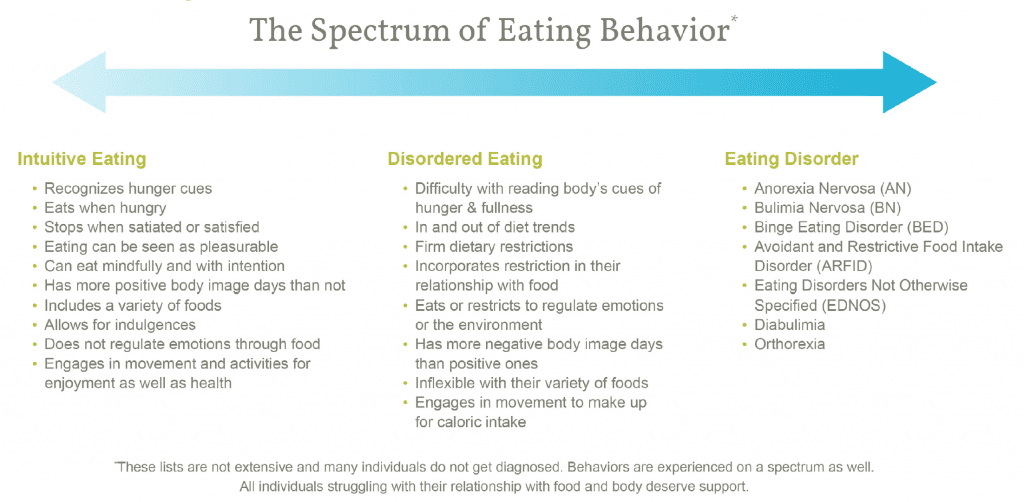
What’s the difference between disordered eating and an Eating Disorder?
- Disordered eating encompasses a set of different behaviors that people may have with food that aren’t healthy. It could be anything from restricting intake, bingeing, overexercising, or manipulating their food to try to lose weight. These may or may not qualify or meet diagnosis for an Eating Disorder, but still are harmful to health. Disordered behaviors may or may not progress into an eating disorder, but it’s helpful to seek support if you do struggle with behaviors to prevent them from getting worse. *JUST because you may not meet criteria for an Eating Disorder does NOT mean you don’t deserve help and support!
- Eating Disorders are serious yet treatable mental and physical illnesses (bio-psycho-social disorders) that can affect people of all genders, ages, races, religions, ethnicities, sexual orientations, body shapes, and weights. National surveys estimate that 20 million women and 10 million men in America will have an eating disorder at some point in their lives. They are diagnosed by certain criteria in the Diagnostic and Statistical Manual of Mental Disorders (or DSM–5). The different Eating Disorder Diagnoses include:
- Anorexia Nervosa (AN)
- Restriction of energy intake relative to requirements leading to a significantly low body weight in the context of age, sex, developmental trajectory, and physical health.
- Intense fear of gaining weight or becoming fat, even though underweight.
- Disturbance in the way in which one’s body weight or shape is experienced, undue influence of body weight or shape on self-evaluation, or denial of the seriousness of the current low body weight.
- Bulimia Nervosa (BN)
- Recurrent episodes of binge eating. An episode of binge eating is characterized by both of the following:
- Eating, in a discrete period of time (e.g. within any 2-hour period), an amount of food that is definitely larger than most people would eat during a similar period of time and under similar circumstances.
- A sense of lack of control over eating during the episode (e.g. a feeling that one cannot stop eating or control what or how much one is eating).
- Recurrent inappropriate compensatory behavior in order to prevent weight gain, such as self-induced vomiting, misuse of laxatives, diuretics, or other medications, fasting, or excessive exercise.
- The binge eating and inappropriate compensatory behaviors both occur, on average, at least once a week for three months.
- Self-evaluation is unduly influenced by body shape and weight.
- The disturbance does not occur exclusively during episodes of anorexia nervosa.
- Recurrent episodes of binge eating. An episode of binge eating is characterized by both of the following:
- Binge Eating Disorder (BED)
- The most common eating disorder.
- Recurrent episodes of binge eating. An episode of binge eating is characterized by both of the following:
- Eating, in a discrete period of time (e.g., within any 2-hour period), an amount of food that is definitely larger than what most people would eat in a similar period of time under similar circumstances.
- A sense of lack of control over eating during the episode (e.g., a feeling that one cannot stop eating or control what or how much one is eating).
- The binge eating episodes are associated with three (or more) of the following:
- Eating much more rapidly than normal.
- Eating until feeling uncomfortably full.
- Eating large amounts of food when not feeling physically hungry.
- Eating alone because of feeling embarrassed by how much one is eating.
- Feeling disgusted with oneself, depressed, or very guilty afterward.
- Marked distress regarding binge eating is present.
- The binge eating occurs, on average, at least once a week for 3 months.
- The binge eating is not associated with the recurrent use of inappropriate compensatory behaviors (e.g., purging) as in bulimia nervosa and does not occur exclusively during the course of bulimia nervosa or anorexia nervosa.
- Avoidant and Restrictive Food Intake Disorder (ARFID)
- An eating or feeding disturbance (e.g., apparent lack of interest in eating or food; avoidance based on the sensory characteristics of food; concern about aversive consequences of eating) as manifested by persistent failure to meet appropriate nutritional and/or energy needs associated with one (or more) of the following:
- Significant weight loss (or failure to achieve expected weight gain or faltering growth in children).
- Significant nutritional deficiency.
- Dependence on enteral feeding or oral nutritional supplements.
- Marked interference with psychosocial functioning.
- The disturbance is not better explained by lack of available food or by an associated culturally sanctioned practice.
- The eating disturbance does not occur exclusively during the course of anorexia nervosa or bulimia nervosa, and there is no evidence of a disturbance in the way in which one’s body weight or shape is experienced.
- The eating disturbance is not attributable to a concurrent medical condition or not better explained by another mental disorder. When the eating disturbance occurs in the context of another condition or disorder, the severity of the eating disturbance exceeds that routinely associated with the condition or disorder and warrants additional clinical attention.
- An eating or feeding disturbance (e.g., apparent lack of interest in eating or food; avoidance based on the sensory characteristics of food; concern about aversive consequences of eating) as manifested by persistent failure to meet appropriate nutritional and/or energy needs associated with one (or more) of the following:
- Other Specified Feeding or Eating Disorder (OSFED) – previously referred to as “EDNOS”
- Atypical Anorexia Nervosa: All criteria are met, except despite significant weight loss, the individual’s weight is within or above the normal range.
- Binge Eating Disorder (of low frequency and/or limited duration): All of the criteria for BED are met, except at a lower frequency and/or for less than three months.
- Bulimia Nervosa (of low frequency and/or limited duration): All of the criteria for bulimia nervosa are met, except that the binge eating and inappropriate compensatory behavior occurs at a lower frequency and/or for less than three months.
- Purging Disorder: Recurrent purging behavior to influence weight or shape in the absence of binge eating.
- Night Eating Syndrome: Recurrent episodes of night eating. Eating after awakening from sleep, or by excessive food consumption after the evening meal. The behavior is not better explained by environmental influences or social norms. The behavior causes significant distress/impairment. The behavior is not better explained by another mental health disorder (e.g. BED).
- Orthorexia (note: orthorexia is not recognized yet by the DSM-5).
- The term ‘orthorexia’ was coined in 1998 and means an obsession with pure or ‘healthful’ eating. Although being aware of and concerned with the nutritional quality of the food you eat isn’t a problem in and of itself, people with orthorexia become so obsessed and fixated on so-called ‘healthy eating’ that they actually become unhealthy. This has become more and more apparent in recent years and more research is needed, as there are aspects of other eating disorders seen in orthorexia that overlap.
- Anorexia Nervosa (AN)
Eating Disorders can greatly affect physical, mental, and emotional health and require treatment from a team of healthcare providers including a physician, registered dietitian, psychiatrist, and therapist. Anorexia Nervosa is the most fatal of ALL mental illnesses. Treatment options range from inpatient hospitalization, residential treatment, PHP (partial hospitalization program), to IOP (intensive outpatient), and outpatient.
source: healthlinkscertified.org
What is normal eating / having a healthy relationship to food look like?
- eating in response to internal cues such as hunger, fullness, & satisfaction
- enjoying a variety of foods, and allowing for fun foods
- not choosing your food choices on its ability to influence your weight
- engaging in movement for health and enjoyment rather than focus on shape/size
- eating is pleasurable and joyful
- can engage in mindfulness with eating
- no guilt or shame with foods
- eating mainly for physical reasons, rather than emotional
- positive body image
- putting some, but not too much, focus on food
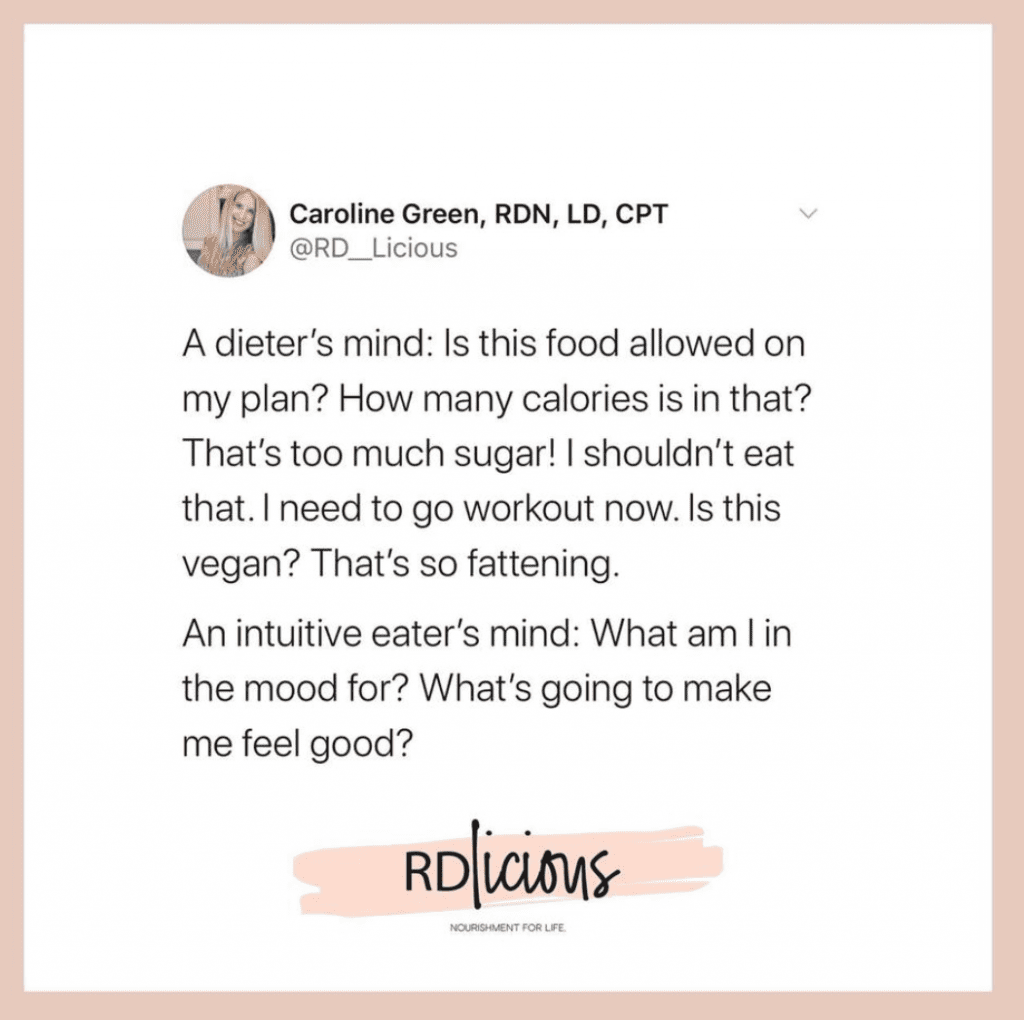
What does it typically feel like once you’ve gotten there?
No crazy external noise 24/7 telling you if you’ve ‘passed’ or ‘failed’ today. No labeling or thinking “is this good? Should I be eating this? Is this vegan? Paleo? Non-GMO? Is this going to make me gain weight?”
It looks like room to think about other things besides food (yay for hobbies! relationships! career!)⠀⠀⠀⠀
It looks like trusting your body that it will make up for mistakes in your eating because our bodies crave balance and a variety of nutrients and we can learn to listen to what it needs.
⠀⠀⠀⠀⠀⠀ ⠀ ⠀⠀
It means learning to cope with your emotions using other things besides food, like taking a bath, going to yoga, or going to bed early instead if that’s what you need, but also not feeling guilt if sometimes you want to eat emotionally, too.
⠀⠀⠀⠀⠀⠀ ⠀ ⠀⠀
It looks like going to the farmers market to get some crisp, fresh produce, but also enjoying some fries with friends without guilt because that’s healthy, too. ⠀⠀⠀⠀⠀⠀ ⠀ ⠀⠀
It means giving less thought to your weight because you understand that it doesn’t tell you much at all about your health. ⠀⠀⠀⠀⠀⠀ ⠀ ⠀⠀
It means fueling your body with a wide variety of foods, and that a zoomed out pattern of eating is what truly matters, not specific nutrients or food choices in that one moment.
⠀⠀⠀⠀⠀⠀ ⠀ ⠀⠀
It looks like giving some, but not all of your day giving too much thought to food, and focusing on other areas of life that are important: your values, your morals, your hobbies, your relationships, your job, your spirituality, and SO much more. ⠀⠀⠀⠀⠀⠀ ⠀ ⠀⠀
Freedom from diet culture and becoming an intuitive eater simply put is PEACEFUL.
⠀⠀⠀⠀⠀ ⠀ ⠀⠀
So…how do you get there if you think you have an unhealthy relationship to food?
Work with a Registered Dietitian who specializes in Intuitive Eating & HAES. Work through the principles. Unfollow social media accounts that promote dieting or speak diet culture. Speak to your body with kindness and respect. Eat regularly, start to pay attention (and trust) your internal hunger & fullness cues. Challenge your ingrained diet beliefs and thoughts. It’s possible and an incredible transformation that’s worth it. YOU are worth it. ????✨
Get My 20 Favorite Recipes!
Get ready for some yummy food with my 20 favorite recipes. Receive an instant download to inspire you on your journey to nourishment!
Follow me on Instagram!
@CAROLINEGREENNUTRITION