Trauma, The Nervous System, and Eating Disorders: The Role of Nutrition Therapy in Treatment
Trauma can have a profound impact on an individual’s mental and physical health, particularly on the nervous system. The way our bodies respond to stress and trauma can affect our eating behaviors and whether we feel safe or not to eat with ease. Trauma can absolutely contribute to the development of eating disorders, as a coping mechanism for disconnecting with the body or managing uncomfortable emotions. Let’s explore the relationship between trauma, the nervous system, and eating disorders, and how nutrition therapy can play a role in treatment.
The Link between Trauma and Eating Disorders
Trauma can take many forms, including physical, sexual, emotional abuse, neglect, and other traumatic experiences. Trauma can lead to changes in the brain and the body’s stress response system, resulting in symptoms such as anxiety, depression, and post-traumatic stress disorder (PTSD). The impact of trauma can also affect a person’s relationship with food and body image, leading to the development of eating disorders such as anorexia nervosa, bulimia nervosa, and binge eating disorder.
Research has shown that individuals who have experienced trauma are at a higher risk of developing an eating disorder. For example, a study by the National Eating Disorders Association found that women with a history of childhood abuse were four times more likely to develop an eating disorder than those without such a history. Additionally, the Adverse Childhood Experiences (ACE) study found that individuals who experienced four or more types of childhood trauma were more likely to engage in disordered eating behaviors. Additionally, here are some statistics from some of Dr. Timothy Brewerton’s studies, who is a well-known expert in the field of trauma and eating disorders:
In a study of 501 patients with eating disorders, 84% reported experiencing at least one type of traumatic event in their lifetime.
Among individuals with eating disorders, those with a history of trauma had significantly higher rates of comorbid psychiatric disorders, including depression, anxiety, and substance use disorders.
In a study of 208 women with anorexia nervosa, 71% reported a history of at least one traumatic event. Among those who reported trauma, 61% reported experiencing multiple traumas.
In a study of 179 women with bulimia nervosa, 75% reported a history of at least one traumatic event. Among those who reported trauma, 69% reported experiencing multiple traumas.
In a study of 290 patients with binge eating disorder, 48% reported a history of at least one traumatic event.
The Role of the Nervous System in Eating Disorders
The nervous system plays a critical role in regulating our body’s response to stress and trauma. When faced with a threat, our body activates the “fight or flight” response, which triggers a surge of stress hormones such as cortisol and adrenaline. These can be helpful in the short term when exposed to danger, like being face-to-face with a bear, to help us run away. But long-term, our nervous system can almost get “stuck” and always be hypervigilant, even when there is no present danger. This response can impact our appetite, our ability to regulate our emotions, and our ability to feel at ease with food.
In individuals who have experienced trauma, the stress response system can become dysregulated, leading to chronic activation of the “fight or flight” response, or even “freeze” response. This can lead to changes in appetite regulation, food intake, and metabolism, which can contribute to the development of eating disorders. The eating disorder becomes the “protector” or a defense strategy, when everything feels like “too much” or “not enough”. Additionally, dysregulation of the stress response system can impact the brain’s reward system, leading to compulsive and addictive behaviors around food at times.
Typically humans fluctuate between three areas of nervous system regulation: hyper-arousal, hypo-arousal, or in between in our Window of Tolerance.
Hyper-arousal, or fight-or-flight, may show up as: anxiety, feeling “too much”, panic, hypervigilence, racing heart, wanting to run away, fidgeting, etc.
Hypo-arousal, or freeze, may show up as: feeling numb, emotionless, fatigue, depression, dissociated, feeling heavy, flat affect.
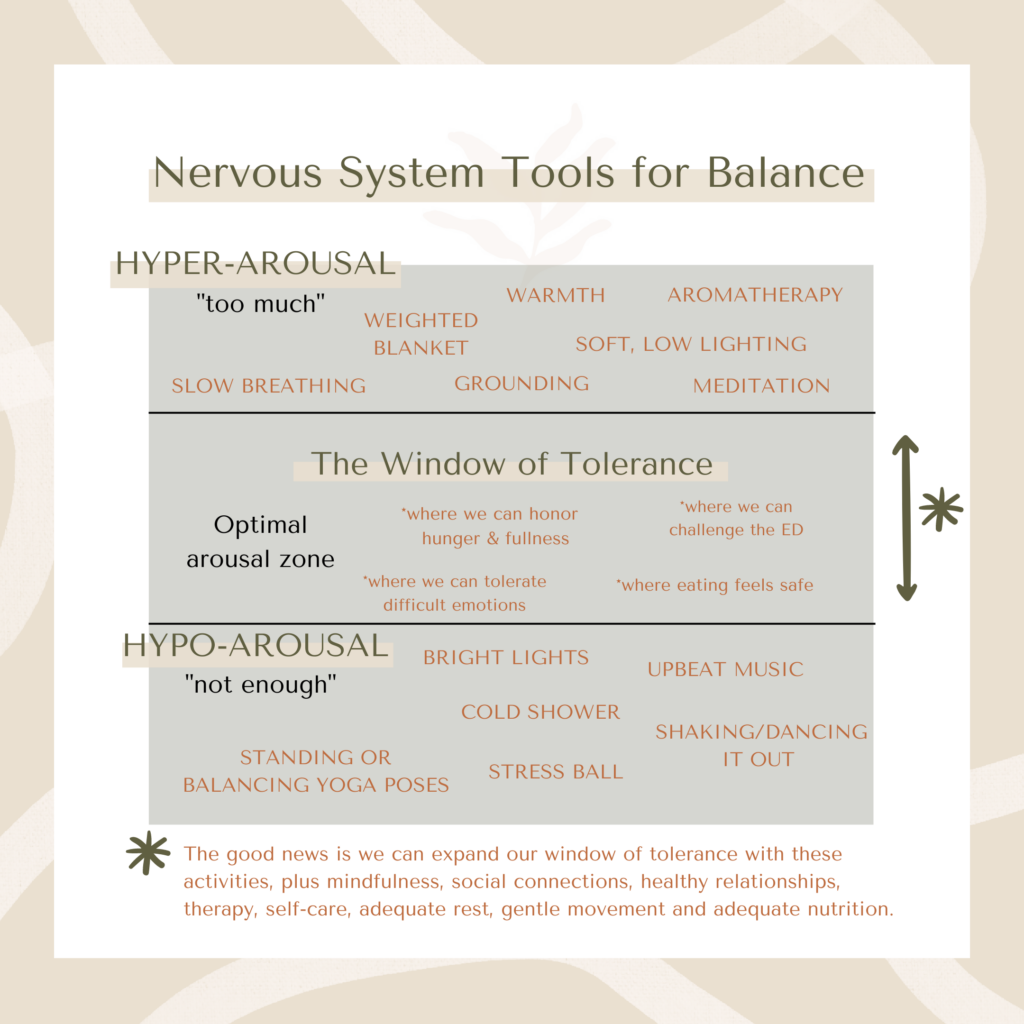
Window of Tolerance (a term coined by Dan Siegel), is the middle-ground where we feel calm, balanced, and we’re able to regulate and process emotions. This is where we feel safe. In individuals who have experienced trauma, the window of tolerance shrinks, therefore its easy to get pushed out and into a hyper- or hypo- state and never feel calm enough to process emotions, sit safely through eating exposures, and more.
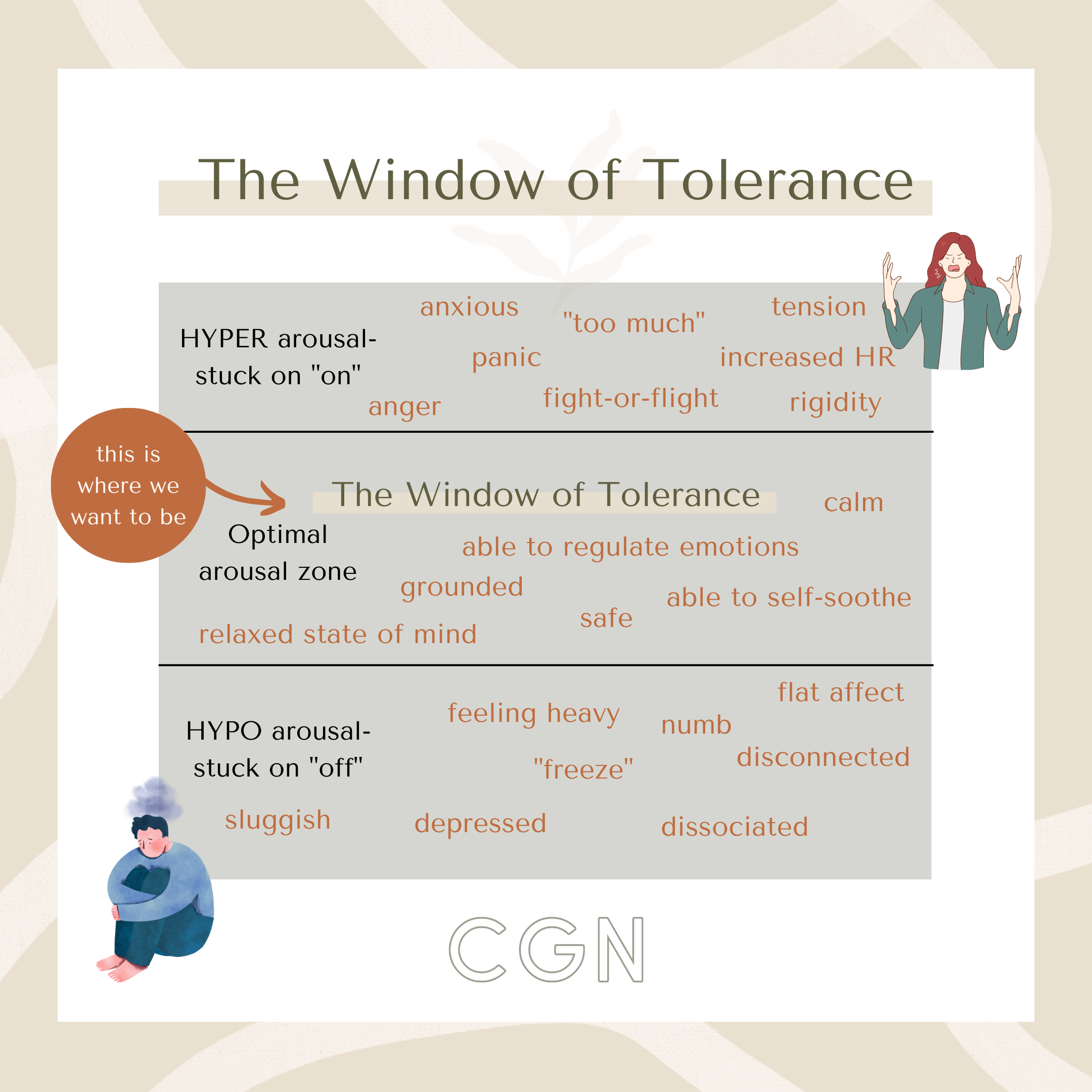
When we are either over-activated or under-activated, we may turn to food behaviors (restriction, food rules, bingeing, overexercise) to try to manage uncomfortable emotions, but it only provides a false sense of safety. But because you feel *slightly less bad*, you continue to engage in your ED behaviors to try to feel better. This creates a vicious cycle, without actually helping you get back to your window of tolerance.
The Role of Nutrition Therapy in Treatment
Somatic Nutrition therapy is an essential component of eating disorder treatment, particularly for individuals who have experienced trauma. The goal of nutrition therapy is to restore and improve physical health, promote normal eating behaviors, and use the body as a resource to let go of stored unprocessed emotions. It can be thought of as using a “Bottom up” approach to treatment, rather than just a “top down” approach through the mind/talk therapy. By incorporating both in my practice we see more long-term progress than using the brain alone. The body holds onto stored memories and tells us alot- so why not bring it into treatment?
In working with individuals who have experienced trauma, it’s imperative that they work through both the trauma and the eating disorder. If the eating disorder is a symptom of trauma, then we have to work at the deeper trauma for long-term recovery. Successful eating disorder treatment should include a trauma component with a trauma-informed therapist on the team. There are quite a few trauma treatment modalities such as: EMDR (Eye Movement Desensitization and Reprocessing), Cognitive Processing Therapy (CPT), Somatic Experiencing, Cognitive Behavioral Therapy (CBT), and Prolonged Exposure. As a Dietitian training in somatics, I cannot recommend somatic experiencing enough, especially for individuals with co-occuring trauma and eating disorders. Find a Somatic Experiencing therapist here.
Additionally, nutrition therapy can help to address the impact of trauma on eating behaviors and body image. This may include developing coping skills to manage anxiety and stress, exploring the connection between emotions and eating behaviors, and addressing any negative beliefs or attitudes towards food and body image using talk therapy. We also slowly, as the client is comfortable and ready, start to tune back into the body by listening to hunger, fullness, and satisfaction. Trauma usually pushes an individual to disconnect from their body, so we must come home to the body for long-term recovery.
Nutrition therapy can also be used to address the dysregulation of the stress response system. This may include incorporating stress-reducing practices such as mindfulness and relaxation techniques, nervous system resources such as weighted blankets, body scans, deep breathing, etc.
Overall, trauma can have a significant impact on the nervous system, leading to changes in eating behaviors and contributing to the development of eating disorders. Nutrition therapy using talk therapy, meal planning, psychoeducation, somatic coaching, and more is an essential component of eating disorder treatment, particularly for individuals who have experienced trauma. By addressing the physical and emotional impact of trauma, supporting normal eating behaviors, and addressing the dysregulation of the stress response system, nutrition therapy can play a critical role in long-term healing using a “bottom up” approach.
Need support for an eating disorder with co-occurring trauma? Reach out today for care.
Get My 20 Favorite Recipes!
Get ready for some yummy food with my 20 favorite recipes. Receive an instant download to inspire you on your journey to nourishment!
Follow me on Instagram!
@CAROLINEGREENNUTRITION