What is polyvagal theory and what the heck does it have to do with eating disorders?
Polyvagal theory, developed by Dr. Stephen Porges, is a framework that helps us understand the role of the autonomic nervous system (ANS) in regulating our physiological and emotional responses to stress and social interactions. While the theory itself does not directly address eating disorders, it provides helpful insights into the underlying mechanisms that may contribute to the development and driver of EDs.
Eating disorders, such as anorexia nervosa, bulimia nervosa, and binge eating disorder, are complex bio-psycho-social conditions that involve a combination of factors. While there is no single cause, it is believed that dysregulation of the autonomic nervous system and emotional dysregulation can play a role in the onset and maintenance of these disorders.
In very simple terms, polyvagal theory describes the autonomic nervous system in 3 parts. These parts influence our involuntary actions (outside of our cognitive control). Our nervous system involves three adaptive responses – one for safety, another for danger, and the other for extreme threat to life. Also known as fight/flight, safety, or freeze/shutdown. These responses are mediated by the vagus nerve, the longest nerve in the body, and each is activated by what we perceive to be happening around and within us at any given moment. Sympathetic system involves our fight/flight, ventral vagal complex is safety, and dorsal vagal complex is shutdown. All three of these states can be somewhat active (to varying degrees) in our nervous system at different times. Moving through the different states can be imagined like a dimmer light switch, it’s not just “on” or “off” but rather nuanced.
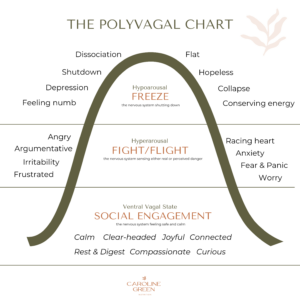
This ventral vagal state is also known as the social engagement system, because this is where we feel calm, connected, able to engage in relationship, and think normatively. Our aim is to get HERE more, to be able to challenge the ED and eat with more ease. If we don’t try to address our nervous system, we’ll just be white-knuckling recovery, and the potential to just retraumatize the system. We want to be able to calm the nervous system, to teach it and rewire it that food can be eaten safely and its not a threat.
In short, nervous stem state impacts eating and digestion. A felt sense of safety (neurobiologically) is needed to support normative eating and digestion.
With trauma, an individual may perceive the world as dangerous, because that has been their experience. They may have a hard time finding or staying in “Safety”, or ventral vagal, due to a variety of reasons (attachment ruptures/no safe person to co-regulate, traumatic events, PTSD etc.) Therefore it is more often difficult to regulate emotions, and they may oscillate between being TOO activated or TOO undertactivated. But there is alwayshope! Working with a trained therapist and a trauma-informed dietitian can help individuals learn about their nervous system states, their learned neural pathways for defensive mechanisms, and how to expand their window of tolerance and regulate.
We know that eating disorders are very often correlated with trauma. Research suggests that trauma exposure rates among individuals with eating disorders range from 30% to 80%, depending on the population studied and the specific type of trauma examined.
The hyperactivated state or hypoactivated state can contribute to disordered eating behaviors as a way to cope with or control these overwhelming emotions and feelings. Going through trauma makes an individual more sensitive to triggers and can make their nervous system be on “high alert”, always on the edge of its seat trying to detect and avoid danger. This makes someone’s nervous system more sensitive to going into activation or shutdown, so its harder to stay in the calm, safe zone aka ventral vagal system.
Most individuals who experience eating issues have a hard time regulating emotions and staying in this state of safety with their nervous system, therefore learning how to regulate the nervous system and anchor to safety can be a vital part of treatment and recovery. Using eating disorder behaviors like restriction, bingeing, or compulsive exercise act as “faux” regulators because they perceive to be helping an individual feel safer/regulate, and yet its not ACTUALLY helping their nervous system to regulate.

So part of what I find integral to eating disorder treatment is teaching clients about their nervous system, how it affects their behaviors around food and body image, and how to practice new, healthier coping skills to regulate their nervous system. For example, did you know deep exhalation breaths help turn the parasympathetic nervous system on, to bring your system back to calm? Which is why slow deep breathing and meditation are some of my favorite coping tools. Breathwork is free, accessible, and easy to use when your system feels activated. There are so many other skills to use to help regulate the nervous system and tap into the vagus nerve, such as yoga, tai chi, essential oils, humming, singing, laughing, soft textures, certain sounds and sensory profiles, ice on the face, and facial massages.
All in all, understanding our fluctuating nervous system states helps us better understand ourselves, our bodies, our ED and coping behaviors, and can help take some of the shame out of engaging in ED behaviors – it makes so much sense you’d be using your ED to try to get back to safety, and yet there are healthier ways that can actually help you reach safety and calm.
Work with a team of trauma-informed professionals if you suffer from an eating disorder and a history of trauma. You deserve healing and support. ♡
Get My 20 Favorite Recipes!
Get ready for some yummy food with my 20 favorite recipes. Receive an instant download to inspire you on your journey to nourishment!
Follow me on Instagram!
@CAROLINEGREENNUTRITION
